CONFRONTING PICTURE OF GROWING WOMEN’S HEALTH CRISIS IN UTERINE CANCERS. ANZGOG State of the Nation report highlights inequities in uterine cancer outcomes across Australia
With
Associate Professor Yoland Antill, Director and Deputy Chair, Australia New Zealand Gynaecological Oncology Group (ANZGOG)
SEGMENT
Filmed in Melbourne | December 2025
Uterine cancers have become Australia’s fastest-growing women’s cancer, with incidence doubling over the past 25 years and projected to continue to surge. Without immediate action, more than 44,000 women are expected to be diagnosed by 2035, and 8,900 will lose their lives to the disease.
Released November 2025, Australia’s first State of the Nation: Uterine Cancers in Australia 2025 report by the Australia New Zealand Gynaecological Oncology Group (ANZGOG), reveals a confronting picture of a growing women’s health crisis that has gone largely unseen and one that now requires immediate, coordinated national action.
Once considered a cancer that primarily affected older women, the report highlights an alarming new trend: incidence is now rising fastest among women aged 25 to 44, with cases in this age group expected to increase by around 60 per cent alone, over the next decade.
Despite its growing impact, uterine cancer remains largely invisible in Australia’s cancer conversation. The limited research available notes, 94 per cent of women are unaware of what uterine or endometrial cancers are yet increased awareness of the disease and risk factors could prevent up to 60 per cent of future diagnoses. Research investment for uterine cancers lags far behind other cancers.
In addition, support and psychosocial care for women living with uterine cancers are inconsistent, and currently there is no dedicated national advocacy organisation. Many women face pain, fatigue, anxiety and long-term side effects alone.
State of the Nation report sets out a national plan to reverse the rise in uterine cancers and transform outcomes for Australian women
The report identifies five urgent priorities: halve incidence, eliminate inequities, ensure access to precision care, support every woman to live well, and invest in research and data. Achieving these goals will require united action from government, researchers, clinicians, industry and the community to deliver the innovation, equity and support Australian women deserve.
Source: Adapted from ANZGOG media release November 2025
Report: ANZGOG State of the Nation Report into Uterine Cancers can be read here https://www.anzgog.org.au/sotn-uterine-cancer, prepared by Insight Economics
You Might also like
-
Global GP Conference comes to Australia
Over 3000 delegates from around the World will gather at the 50th celebration of WONCA to reconnect and revive General Practice, sharing knowledge and learnings on access, equity, funding, and multidisciplinary care teams. This includes networking with Australian and overseas GPs and in particular learning about primary care practices in other countries.
Australian Health Journal met with Dr Nicole Higgins, President of RACGP in transit at Brisbane Airport recently and she spoke about the $6 Billion allocated in the Federal Budget in May as a significant achievement for General Practice investment. She also emphasised this announcement reinforced GPs should be at the centre of multidisciplinary care teams to ensure continuity of care and better health outcomes.
-
Inaugural vaccine value chain conference talks about Team Australia
For the first time, key decision-makers and thought leaders from government, industry, academia, NGOs, and representatives from the immunisation community converged in a 2 day conference in Sydney hosted by Biointelect, highlighting the transformative potential of collaborative innovation.
-
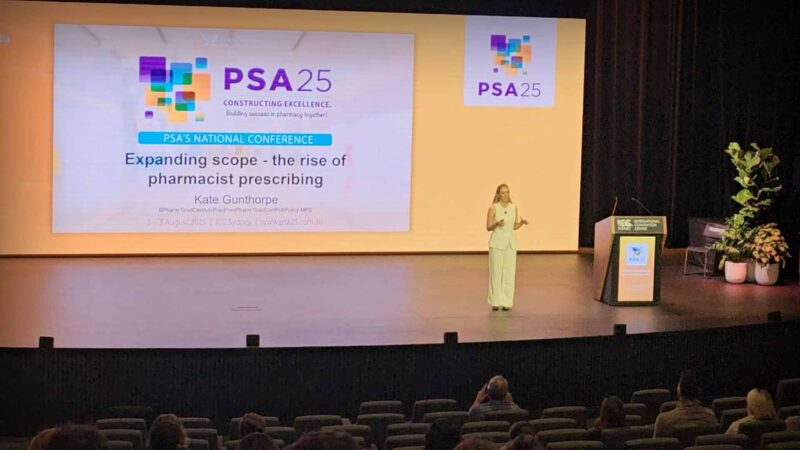
Pharmacist Prescribing Model gets further support from state health
A full scope pharmacist prescriber model allows pharmacists to independently prescribe medicines within their professional competence, without requiring prior doctor authorisation. It extends pharmacists’ role beyond dispensing to include assessment, diagnosis of minor and chronic conditions, initiation and modification of therapy, and ongoing patient monitoring. This model integrates pharmacists into primary care teams, aiming to improve timely access to treatment, reduce pressure on general practitioners, and enhance continuity of care. Pharmacists use their clinical knowledge, patient records, and collaborative pathways to ensure safe prescribing. The model emphasises training, regulation, and accountability to maintain high standards of patient safety.