Collaboration between industry, research, universities, government, and organisations is crucial for vaccine development and addressing public health needs, with a focus on overcoming barriers, accelerating access to technologies, and enhancing public-private partnerships. This is emphasised by the program committee chair Jenny Herz and a program committee member Professor Jodie McVernon of the Inaugural Vaccine Value Chain Conference, who invited Australian Health Journal to attend.
For the first time, key decision-makers and thought leaders from government, industry, academia, NGOs, and representatives from the immunisation community converged in a 2 day conference in Sydney hosted by Biointelect, highlighting the transformative potential of collaborative innovation.
In talking to Australian Health Journal, Ms Herz spoke about the end to end value chain of vaccine development involving discovery, research, product development, clinical trials, regulatory and reimbursement processes, and community implementation, with a focus on understanding the community’s perspectives and needs. Collaboration between industry and academic research is crucial for overcoming challenges in vaccine development and commercialisation.
She reflects how the pandemic spurred innovation in vaccine development and clinical trials, revealing the need to address gaps and explore new pathways for accelerating access to technologies and medicine, with more venture capital available for funding oncology products than infectious diseases.
According to the Inaugural Program Committee, there are many aspects involved in the value chain of vaccines from discovery through to implementation. However, the understanding of all the challenges, barriers, and levers to streamline the value chain across all key stakeholders is fragmented and sometimes siloed in Australia’s federated system.
During the COVID-19 pandemic novel vaccines were developed globally in record time. Australia’s public health ecosystem pulled together, but the gaps became clear. Since then, there have been many lessons learnt and significant investment by jurisdictional and Federal Governments, the private sector and philanthropy into different parts of the ecosystem.
While Australia has strengths in many areas, such as discovery research, the knowledge and experience to translate discoveries effectively, to truly impact the health of the community, requires data availability, resources and know-how all along the value chain. Access to funding and skilled workforce remains fragmented across our ecosystem, and this affects Australia’s ability to capitalise on research strengths in infectious diseases and immunology.
Professor McVernon and Ms Herz talk about collaboration between public and private sectors being essential to address unmet needs, and funding for innovation to come from NGOs, philanthropy, or public money if it is not attractive to the private sector.
The consensus of opinions coming from the conference speakers and delegates was that Australia needs to take a national approach and present itself as a strong player in the international community to find its relevant place in the value chain.
You Might also like
-
Budget22 A mixed dose of health outcomes
Australian Health Journal met with a number of industry heads after the budget on their journeys so far in lobbying for change, their achievements, some of the disappointments and their thoughts on the road ahead, with an election round the corner.
-
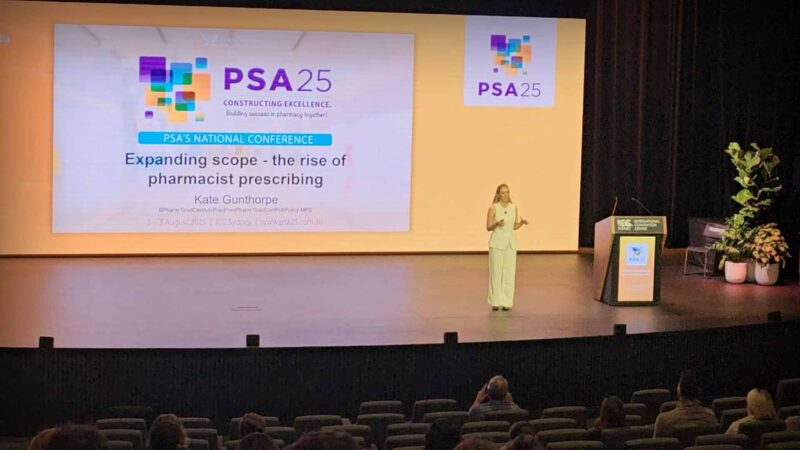
Pharmacist Prescribing Model gets further support from state health
A full scope pharmacist prescriber model allows pharmacists to independently prescribe medicines within their professional competence, without requiring prior doctor authorisation. It extends pharmacists’ role beyond dispensing to include assessment, diagnosis of minor and chronic conditions, initiation and modification of therapy, and ongoing patient monitoring. This model integrates pharmacists into primary care teams, aiming to improve timely access to treatment, reduce pressure on general practitioners, and enhance continuity of care. Pharmacists use their clinical knowledge, patient records, and collaborative pathways to ensure safe prescribing. The model emphasises training, regulation, and accountability to maintain high standards of patient safety.
-
Paramedics seek team-based primary health care pilots
The Chief Executive Officer of The Australasian College of Paramedicine, John Bruning spoke with Australian Health Journal about the following:
New models of care proposed for paramedics
Paramedicine pilot program in the pre-budget submission
Scope of how paramedics can support General Practice, and guidelines on safety and quality
Current limitations experienced by paramedics needing to be addressed by Government
Other health priorities hopefully addressed in Federal Budget.In the lead up to the Australian Federal Budget in May 2023, Australian Health Journal reached out to peak health industry bodies to hear about their priorities, either noted in pre-budget submissions lodged with Federal Government in January 2023 or in recent forums such as the Strengthening Medicare Taskforce.