Social isolation refers to limited social contact and interaction with others, resulting in feelings of loneliness and disconnection. It disproportionately affects the elderly due to factors like loss of friends and family, retirement, reduced mobility, ageism, and limited access to technology. The elderly are at higher risk of social isolation as they may experience a shrinking social circle and face barriers to social participation. Social isolation has significant detrimental effects on their mental and physical well-being, leading to increased rates of depression, anxiety, cognitive decline, and reduced quality of life. Addressing social isolation among the elderly is crucial for promoting their overall health and happiness.
Social prescribing is a healthcare approach that recognises the importance of social factors in overall well-being. It involves connecting individuals with non-medical activities and community resources to improve their health and quality of life. Healthcare professionals, such as doctors or social workers, “prescribe” activities like art classes, gardening, exercise groups, or support groups, which can address underlying social determinants of health and promote holistic well-being. By addressing social isolation, mental health, and lifestyle factors, social prescribing aims to enhance individual health outcomes and reduce the burden on healthcare services.
Social prescribing provides support in various areas of people’s lives, leading to increased confidence, improved navigation of systems, and enhanced friendships and trust in healthcare, while communities should be designed in an age-friendly way to prevent isolation.
In Part 1 of the Models of Care on Social Prescribing, Australian Health Journal spoke to 4 people advocating for social prescribing in Australia:
- Dr Michelle Lim, Scientific Chair and Chairperson, Ending Loneliness Together
- Patricia Sparrow, Chief Executive Officer, COTA Australia
- Dr Paresh Dawda, General Practitioner, Director and Principal, Next Practice Deakin. All well as being a UK GP
- Tracey Johnson, Chief Executive Officer, Inala Primary Care
The discussions with these advocates emphasise social prescribing is a necessary solution to address isolation, loneliness, and stress, but it requires more resources, funding, and support to make it accessible and affordable for individuals, particularly older Australians.
You Might also like
-
25 years of non-indexation of nuclear medicine impeding access & affordability
The President of the Australasian Association of Nuclear Medicine Specialists (AANMS), Associate Professor Sze Ting Lee spoke with Australian Health Journal about the following:
Usual levels of nuclear medicine services in Australia each year
Current levels of nuclear medicine services in Australia
How changing demographics in people moving to regional areas has impacted access to nuclear medicine services
The nuclear medicine workforce including trainees
The key recommendations from the pre-budget submissionIn the lead up to the Australian Federal Budget in May 2023, Australian Health Journal reached out to peak health industry bodies to hear about their priorities, either noted in pre-budget submissions lodged with Federal Government in January 2023 or in recent forums such as the Strengthening Medicare Taskforce.
-
From refugee to receiving multiple accolades as a community pharmacist
Sara is an experienced pharmacist, community health advocate, and the Lead Pharmacist at Pharmacy 777 Pascoe Vale in Victoria. With over 20 years in the profession, Sara has played a significant role in advancing local healthcare delivery through clinical leadership, service development, and strong community partnerships.
-
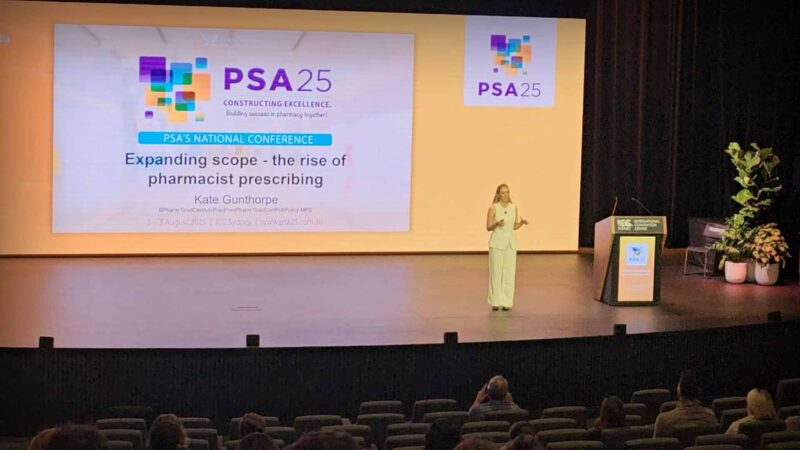
Pharmacist Prescribing Model gets further support from state health
A full scope pharmacist prescriber model allows pharmacists to independently prescribe medicines within their professional competence, without requiring prior doctor authorisation. It extends pharmacists’ role beyond dispensing to include assessment, diagnosis of minor and chronic conditions, initiation and modification of therapy, and ongoing patient monitoring. This model integrates pharmacists into primary care teams, aiming to improve timely access to treatment, reduce pressure on general practitioners, and enhance continuity of care. Pharmacists use their clinical knowledge, patient records, and collaborative pathways to ensure safe prescribing. The model emphasises training, regulation, and accountability to maintain high standards of patient safety.